Bone broth, also known as stock, is recently back in fashion with many purported health benefits. I will admit my own bias in being rather a fan of some good bone broth and suspect it is a beneficial component of the diet, although good research is currently still rather lacking.
However, it is important not to idolise particular foods, as almost all foods have some potential downsides. Therefore, I was interested to find a potential downside to bone broth in the link between broth, gelatine, oxalate, and kidney stones. This may seem unlikely as bone broth does not contain any oxalate, but bear with me as this first requires a diversion into the formation of kidney stones and where oxalate comes from.
Kidney stones
Kidney stones are really quite common, affecting about 1 in 10 people at some point in their lives. Most (~90%) kidney stones are formed of crystals of calcium and oxalate. Crystals of calcium oxalate begin to form when the concentration of calcium and oxalate reaches a high enough concentration. This means that a higher concentration of oxalate in the kidneys is a risk factor for developing kidney stones. As oxalic acid is found in a variety of foods, patients with recurrent kidney stones are often advised to limit their intake of foods containing a lot of oxalate. However, the oxalate from food only makes up a proportion of the oxalic acid in excreted from by the kidney, with estimates of between 24% and 53% originating from the diet (Holmes 2001).
Hydroxyproline metabolism
The rest of the oxalate passing through the kidneys is produced by the body itself. Oxalate is the final step in the breakdown of a common amino acid called hydroxyproline. Collagen is the major structural protein in the body and also the most abundant protein making up from 25% to 35% of all the protein in the body. Mostly found in fibrous tissues such as tendons, ligaments, and skin. It is also abundant in corneas, cartilage, bones, blood vessels, the gut, spinal discs, and the dentin in the teeth. Normally, the collagen in our connective tissues turns over at a very slow and controlled rate and is always slowly being broken down and rebuilt. This constant renewal of collagen requires the body to remove excess amino acids released during the process.
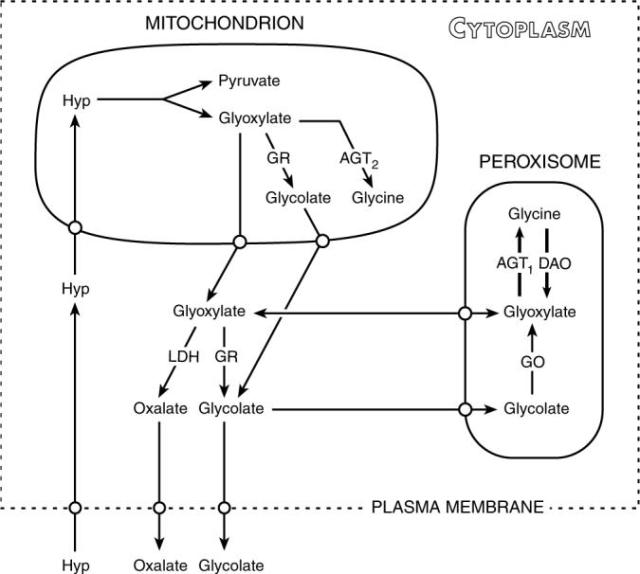
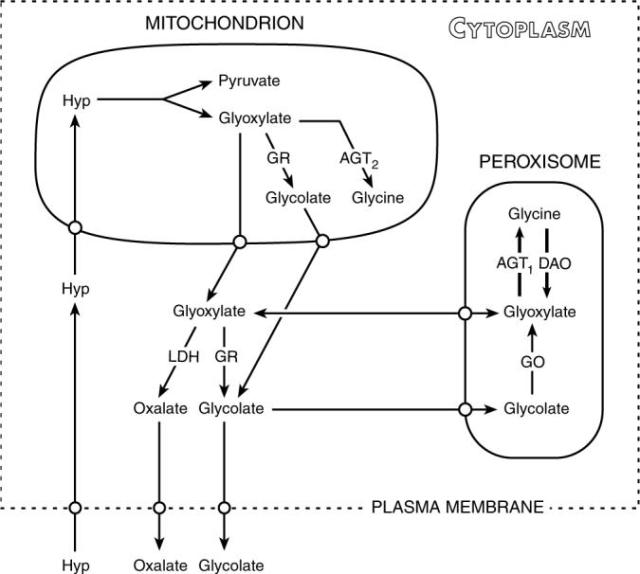
The metabolic pathways of hydroxyproline metabolism into oxalate. Source: (Knight 2006).
The daily turnover of collagen from your own body is a major source of hydroxyproline. Just turning over your own collagen accounts for 5-20% of the urinary oxalate daily (Knight 2006). Excess hydroxyproline goes through a complex metabolic pathway in the liver. The majority of the hydroxyproline in this pathway is actually converted into another amino acid, glycine, and used for other purposes. There remainder is finally converted to oxalic acid and glycolate, which are excreted by the kidneys.
Bone broth gelatine contains hydroxyproline
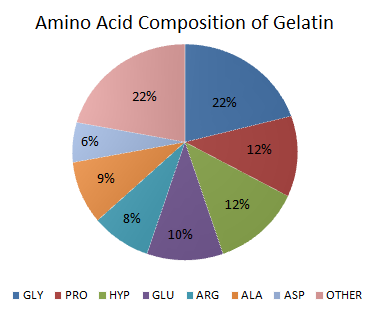
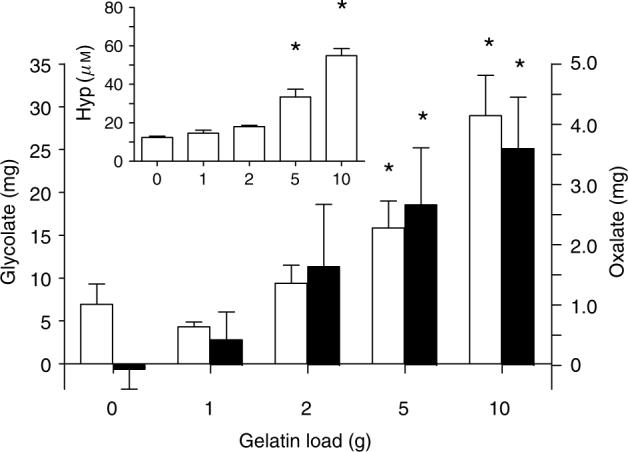
“Amino Acid Composition in Gelatine chart” by Hugahoody
We now return to bone broth of which hydrolysed collagen, better known as gelatine, is the main protein. It is gelatine that makes a good broth gel when cooled and contains the particular composition of amino acids that are currently making broth a popular health food. You can see from the pie chart below that hydroxyproline (Hyp) makes up 12% of the amino acids in gelatine. After eating broth or gelatine the body suddenly has a lot of hydroxyproline to deal with and a proportion of this is converted into oxalate.
A ten gram dose of gelatine increases hydroxyproline in the blood
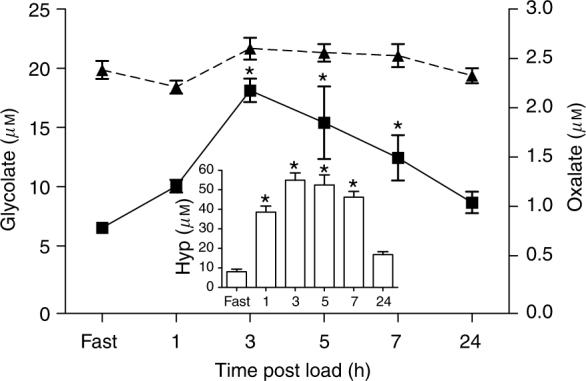
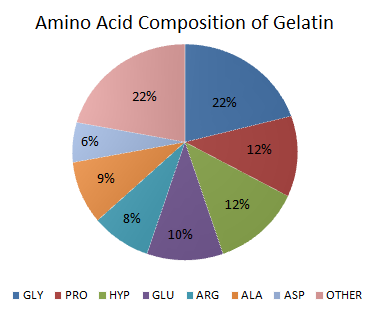
Change in blood hydroxyproline (Hyp) (inset), glycolate (■), and oxalate (–▲–) after ingestion of 10 g of gelatine. Source: (Knight 2006).
When gelatine is consumed there is a rise in the amount of hydroxyproline in the blood for several hours. In a fascinating paper from 2007, John Knight and his colleagues fed ten subjects thirty grams of supplemental gelatine and then measured their blood and urine. From their graph below you can see that the hydroxyproline (Hyp) levels rapidly rose in the blood and remained up to four times higher for several hours. However, oxalate levels in the blood are more tightly controlled and did not rise.
A ten gram dose of gelatine increases oxalate in the urine
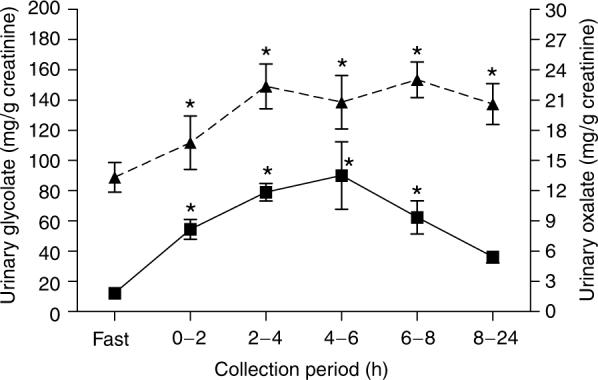
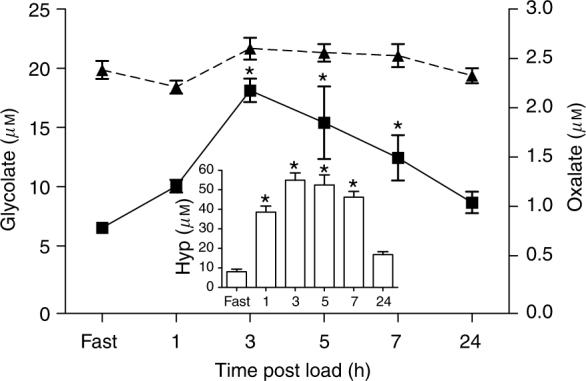
Amount of glycolate (■) and oxalate (–▲–) in the urine following ingestion of 10 grams of gelatine. Source: (Knight 2006).
In comparison, the amount of oxalate in the urine increased for at least eight hours after consuming the gelatine. Oxalate concentration in the urine reached nearly five times higher a few hours after ingesting gelatine. This is due to the kidneys clearing oxalate out of the body as fast as it is being produced. This ten gram dose of gelatine would contain about a gram of hydroxyproline.
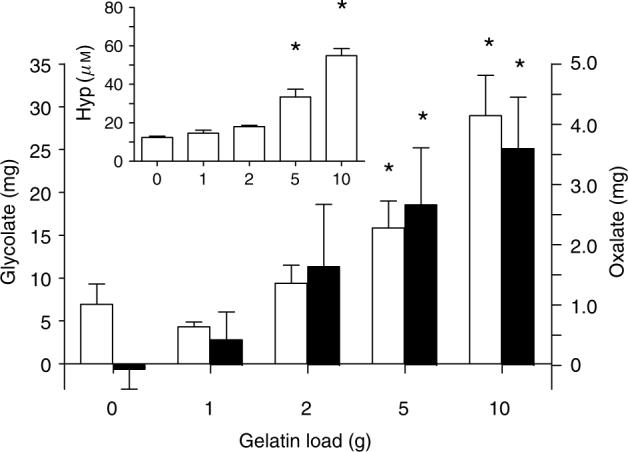
Lower doses of gelatine also increase oxalate in the urine
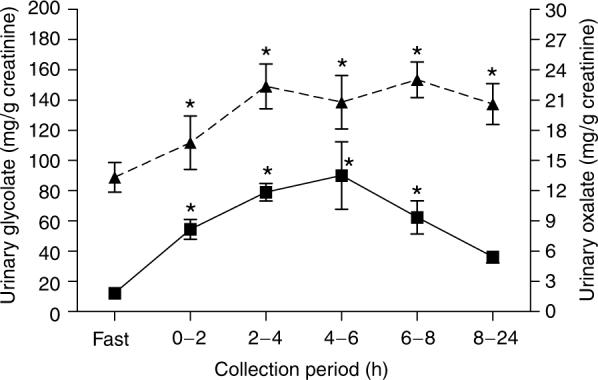
Increases in urinary oxalate (■) and glycolate (□) excretion over fasting levels in a 6 hour period following ingestion of various amounts of gelatine. Source: (Knight 2006).
This is all very well you may say, but ten grams of gelatine is rather more than most people consume in one go. Well, the authors quite rightly followed this up with a range of doses of gelatine more commonly found in the diet. You can see from the graph below that one and two gram doses had little impact on the amount of hydroxyproline. Between five and ten grams of gelatine, there was a significant increase in both hydroxyproline in the blood and oxalate in the urine. Interestingly, 12 grams is the serving of gelatine recommended by a popular geleatine supplement company, just to give perspective on the amounts involved.
Relevance
It would be appropriate now to ask how relevant this information is. There is certainly no study on people who consume bone broth or gelatine regularly and their risk of kidney stones. There is some epidemiological evidence that suggests it may be relevant. This comes from studies comparing meat intake and vegetarians. A recent study has found an association between meat intake and kidney stones, with a significantly reduced risk of stones occurring in vegetarians or people eating less meat (Turney 2014). The hydroxyproline content of meat products is suspected to play a role in this increased risk. Meat is the main source of gelatine in most peoples’ diets and a hundred grams of beef can contain a few grams of collagen. Of course, this cannot be treated as conclusive evidence as it is only an association. In an older study, meat intake – which contains collagen and hydroxyproline – was linked to increasing oxalate excretion, but only in a subgroup of men with unexplained recurrent kidney stones (Nguyen 2001).
Implications
The research presented here is not a intended to scare people away from bone broth, stock, gelatine, or meat. Most people never get kidney stones and even for those who do, there are a number of factors that influence stone development. However, it is a potential factor that may be important for some people to know. As is it not commonly discussed, some people may not make a connection between broth or gelatine intake and kidney stones. If you need to reduce your oxalate levels, caution may be needed when taking extra gelatine or bone broth.
References
Holmes RP, Goodman HO, Assimos DG. (2001) Contribution of dietary oxalate to urinary oxalate excretion. Kidney International. 59(1):270-6.
“BACKGROUND: The amount of oxalate excreted in urine has a significant impact on calcium oxalate supersaturation and stone formation. Dietary oxalate is believed to make only a minor (10 to 20%) contribution to the amount of oxalate excreted in urine, but the validity of the experimental observations that support this conclusion can be questioned. An understanding of the actual contribution of dietary oxalate to urinary oxalate excretion is important, as it is potentially modifiable.
METHODS: We varied the amount of dietary oxalate consumed by a group of adult individuals using formula diets and controlled, solid-food diets with a known oxalate content, determined by a recently developed analytical procedure. Controlled solid-food diets were consumed containing 10, 50, and 250 mg of oxalate/2500 kcal, as well as formula diets containing 0 and 180 mg oxalate/2500 kcal. Changes in the content of oxalate and other ions were assessed in 24-hour urine collections.
RESULTS: Urinary oxalate excretion increased as dietary oxalate intake increased. With oxalate-containing diets, the mean contribution of dietary oxalate to urinary oxalate excretion ranged from 24.4 +/- 15.5% on the 10 mg/2500 kcal/day diet to 41.5 +/- 9.1% on the 250 mg/2500 kcal/day diet, much higher than previously estimated. When the calcium content of a diet containing 250 mg of oxalate was reduced from 1002 mg to 391 mg, urinary oxalate excretion increased by a mean of 28.2 +/- 4.8%, and the mean dietary contribution increased to 52.6 +/- 8.6%.
CONCLUSIONS: These results suggest that dietary oxalate makes a much greater contribution to urinary oxalate excretion than previously recognized, that dietary calcium influences the bioavailability of ingested oxalate, and that the absorption of dietary oxalate may be an important factor in calcium oxalate stone formation.”
Knight J, Jiang J, Assimos DG, and Holmes RP. (2006) Hydroxyproline ingestion and urinary oxalate and glycolate excretion Kidney International. 70(11): 1929–1934.
“Endogenous synthesis of oxalate is an important contributor to calcium oxalate stone formation and renal impairment associated with primary hyperoxaluria. Although the principal precursor of oxalate is believed to be glyoxylate, pathways in humans resulting in glyoxylate synthesis are not well defined. Hydroxyproline, a component amino acid of collagen, is a potential glyoxylate precursor. We have investigated the contribution of dietary hydroxyproline derived from gelatin to urinary oxalate and glycolate excretion. Responses to the ingestion of 30 g of gelatin or whey protein were compared on controlled oxalate diets. The time course of metabolism of a 10 g gelatin load was determined as well as the response to varying gelatin loads. Urinary glycolate excretion was 5.3-fold higher on the gelatin diet compared to the whey diet and urinary oxalate excretion was 43% higher. Significant changes in plasma hydroxyproline and urinary oxalate and glycolate were observed with 5 and 10 g gelatin loads, but not 1 and 2 g loads. Extrapolation of these results to daily anticipated collagen turnover and hydroxyproline intake suggests that hydroxyproline metabolism contributes 20−50% of glycolate excreted in urine and 5−20% of urinary oxalate derived from endogenous synthesis. Our results also revealed that the kidney absorbs significant quantities of hydroxyproline and glycolate, and their metabolism to oxalate in this tissue warrants further consideration.”
Turney BW, Appleby PN, Reynard JM, Noble JG, Key TJ, Allen NE.(2014) Diet and risk of kidney stones in the Oxford cohort of the European Prospective Investigation into Cancer and Nutrition (EPIC).European Journal of Epidemiology. 29(5):363-9.
“The lifetime prevalence of kidney stones is around 10 % and incidence rates are increasing. Diet may be an important determinant of kidney stone development. Our objective was to investigate the association between diet and kidney stone risk in a population with a wide range of diets. This association was examined among 51,336 participants in the Oxford arm of the European Prospective Investigation into Cancer and Nutrition using data from Hospital Episode Statistics in England and Scottish Morbidity Records. In the cohort, 303 participants attended hospital with a new kidney stone episode. Cox proportional hazards regression was performed to calculate hazard ratios (HR) and their 95 % confidence intervals (95 % CI). Compared to those with high intake of meat (>100 g/day), the HR estimates for moderate meat-eaters (50-99 g/day), low meat-eaters (<50 g/day), fish-eaters and vegetarians were 0.80 (95 % CI 0.57-1.11), 0.52 (95 % CI 0.35-0.8), 0.73 (95 % CI 0.48-1.11) and 0.69 (95 % CI 0.48-0.98), respectively. High intakes of fresh fruit, fibre from wholegrain cereals and magnesium were also associated with a lower risk of kidney stone formation. A high intake of zinc was associated with a higher risk. In conclusion, vegetarians have a lower risk of developing kidney stones compared with those who eat a high meat diet. This information may be important to advise the public about prevention of kidney stone formation.”
Nguyen QV, Kälin A, Drouve U, Casez JP, Jaeger P. (2001) Sensitivity to meat protein intake and hyperoxaluria in idiopathic calcium stone formers. Kidney International. 59(6):2273-81.
“BACKGROUND: High protein intake is an accepted risk factor for renal stone disease. Whether meat protein intake affects oxaluria, however, remains controversial in healthy subjects and in stone formers. This study was designed (1) to test the oxaluric response to a meat protein load in male recurrent idiopathic calcium stone formers (ICSFs) with and without mild metabolic hyperoxaluria (MMH and non-MMH, respectively), as well as in healthy controls, and (2) to seek for possible disturbed vitamin B(6) metabolism in MMH, in analogy with primary hyperoxaluria.
METHODS: Twelve MMH, 8 non-MMH, and 13 healthy males were studied after five days on a high meat protein diet (HPD; 700 gmeat/fish daily) following a run-in phase of five days on a moderate protein diet (MPD; 160 g meat/fish daily). In both diets, oxalate-rich nutrients were avoided, as well as sweeteners and vitamin C-containing medicines. Twenty-four-hour urinary excretion of oxalate was measured on the last day of each period, along with 4-pyridoxic acid (U(4PA)) and markers of protein intake, that is, urea, phosphate, uric acid, and sulfate. Serum pyridoxal 5′ phosphate (S(P5P)) was measured after protein loading.
RESULTS: Switching from MPD (0.97 +/- 0.18 g protein/kg/day) to HPD (2.26 +/- 0.38 g protein/kg/day) led to the expected rise in the urinary excretion rates of all markers of protein intake in all subjects. Concurrently, the mean urinary excretion of oxalate increased in ICSFs taken as a whole (+73 +/- 134 micromol/24 h, P = 0.024) as well as in the MMH subgroup (+100 +/- 144 micromol/24 h, P = 0.034) but not in controls (-17 +/- 63 micromol/24 h). In seven ICSFs (4 MMH and 3 non-MMH) but in none of the healthy controls (P = 0.016, chi square), an increment in oxaluria was observed and considered as significant based on the intra-assay coefficient of variation at our laboratory (8.5%). There was no difference in S(P5P)nd U(4PA)etween the groups after protein loading.
CONCLUSION: Approximately one third of ICSFs with or without so-called MMH are sensitive to meat protein in terms of oxalate excretion, as opposed to healthy subjects. Mechanisms underlying this sensitivity to meat protein remain to be elucidated and do not seem to involve vitamin B(6) deficiency.”
If one has leaky gut two main healers to intake is bone broth and hydrolyzed collagen. The leaky gut diet itself also contains large amounts of high oxalate foods. Would it be safe to say, knowing the issues leaky gut presents that one could become increasingly sensitive/allergic to high oxalated foods while trying to heal a leaky gut?
LikeLike
Good stuff, thank you. I suffer from restless leg syndrome and am on a low oxalate diet because many have put it into remission by reducing oxalate intake. I found this article because I just purchased bone both protein and have had three sleepless nights in a row. There are so many variables and possible triggers — but this article leads me to believe it is at least worth eliminating for a few days and logging results. What do you think?
LikeLike
Thanks for the comment, that is an interesting observation.I have not heard of experiences of reduced oxalate helping with restless leg syndrome before.
How much were you taking? It would certainly be worth eliminating for a few days and logging results. I would be interested if you notice any difference.
LikeLike
Excellent summary! Congratulations.
About eleven years ago, after the work I did the previous decade led me into discovering that oxalate was elevated in children with autism, I began to go to international oxalate research conferences. I spent four months before my first conference studying the medical literature that describes how oxalate goes all over the body. This education is why I was very surprised to learn that these conferences were attended only by kidney doctors concerned about kidney stones or they were studying one of three genetic conditions called the primary hyperoxalurias. Those three conditions are caused by a genetic defect that leads to the liver making oxalate. Oxalate formed this way goes all over the body producing a condition called oxalosis.
Because of that disease, which can be fatal,we’ve learned that oxalate is very toxic to cells all over the body and especially to mitochondria, and it even gets into the brain, but nobody was studying this issue since the field was all kidney doctors. Laboratories in the US were unwilling to even measure oxalate in a population that didn’t have kidney stones, so I had to recruit oxalate scientists and researchers in Poland to produce with me the first study on oxalate levels in autism, and you can read it here: http://usautism.org/content/PDF_files_newsletters/oxalate_and_autism.pdf
There were many other diseases where studies had found that oxalate was high, like cystic fibrosis, bariatric surgery. inflammatory bowel diseases, celiac sprue, short bowel syndrome and even Down syndrome, but the literature on them made assumptions that the only problem elevated oxalate would cause was kidney problems. But was that true or was it an assumption?
I set up a yahoo group, and at first it was just for autiam but it would allow parents to see if reducing dietary oxalate would help their children with their autism, and it did, producing improvements both in health and behavioral issues.
Because people live in families, soon we started getting reports of other conditions that improved in other family members by reducing oxalate. Many were pain conditions. In eleven years, that group expanded to include a facebook group. Both were called “Trying Low Oxalates” and they have grown together into serving more than 23,000 people. It is very usual to hear that those reducing oxalate (in time) are reporting significant improvements in chronic conditions.
We recently learned that the innate immunity is triggered into overdrive when phagocytic cells of our immune system are patrolling the body for pathogens.
When they find oxalate crystals in the blood or tissues, taking in those crystals will trigger inflammation by causing the formation of a structure called the inflammasome.
The inflammasome is newly discovered and is spurring a huge academic interest right now. I looked in LinkedIn and found more than a thousand scientists studying this area (but not about oxalate’s role), so we hope when we get funding to understand the role of oxalate in all this that we will learn more about how oxalate is affecting us all over the body.
It is possible the interaction of oxalate with the inflammasome could tweak immunity in a way that is unfavorable. Perhaps such a mechanism explains why we received astonishing results in a poll from our listmates who had autoimmune disease (19 different diseases reported). The majority of them found that reducing oxalate from a high oxalate diet to a low one produced a positive effect on their autoimmune disease. This was only a poll but Info on this and a review of the literature is about to be published, but is now in peer review.
I just wanted to address the issue that the kidneys are not the only issue affected by oxalate. I think it is people who are drinking these broths who will need to figure out if the amount of oxalate generated this way is getting them in trouble, but I hope they will learn how to look for oxalate isssues outside the kidney. Back then, we didn’t know how to recognized oxalate issues in the rest of the body, so we were very surprised by the seriousness of the oxalate issue in autism. We just don’t know how big a problem elevations of oxalate really are in the general population since nobody was measuring it!
For more info, please see http://www.lowoxalate.info and its associated support group. The science keeps growing to help us understand why reducing oxalate has really helped a lot of people.
LikeLiked by 1 person
Ms. Owens-
I owe you so much gratitude! My daughter and I were literally dying from high levels of oxalates. Doctors were unable to diagnose either one of us as we both grew more and more ill. I had legally tried every single diet. Lastly, I put the both of us on a vegan diet and we were worse than ever. I came across an article entitled, “Are Green Smoothies Killing You”. I began to learn about oxalates which lead me to your article regarding autistic children. My daughter was high functioning but had been diagnosed with Aspergers. I was so fascinated by your research and thanked the Lord for finally giving us an answer.
We both were secretly anemic, had boils, terrible immune systems, she had pain and burning during urination, I had kidney pain with he material, her eyeglass prescription was doubling every six months, her teeth were falling out, my blood pressure was through the roof, she was locked in a zombie like state more than not. It felt like I was living with RainMan.
We lowered our oxalates, which was a huge life changer for us, but still I knew we were missing some major component. I came across some information regarding collagen peptides and watched my daughter completely and totally change! Her vision even improved!
Collagen peptides were too harsh for me so I have to use hydrolyzed collagen. It has been amazing for me! I recently started my oldest daughter on the hydrolyzed collagen for severe acne that was just not clearing up with diet. It’s already looking better. Clearly they’re is a leaky gut connection with all of us.
I credit your research to saving mine and my daughter’s life and tell everyone I can!
Your’s sincerely,
Shiloh
LikeLiked by 1 person
Hi Shiloh,
Great post. Just looking into oxolates myself. I’m finding it confusing that the above article says collagen increases urine oxolates but you said adding collagen to your diet after decreasing oxalates is helping you tremendously. Could you please explain more.
I’ve also added 10 gm of collagen to my diet after being floxed and it’s made a big impact on my hair nails and skin. I’m now concerned that I will get kidney stones from it. I had 2 kidney stones decades ago but haven’t had issues since. However a ct scan revealed I’ve a few small ones rattling around in there.
Also what’s the difference between peptides and hydrolyzed? My Google search brings them up as the same.
LikeLike
I’ve read this article and the comments because for the past two weeks I’ve been taking 4 oz. of day of bone broth for gut health. For the past 3 days because I came down with a cold, I upped my dose to 4 oz. twice a day. My cold has been a breeze on the bone broth. However, the two days that I upped my dosage I developed really bad kidney pain. So now I’m going to take a couple days off and then continue again with lower doses and less frequencies. If I feel any more kidney pain, I guess I can’t do bone broth. That would be upsetting because it has helped calm down inflammation in my body.
LikeLike
Hi! I’m so glad to have come across this article. I was experiencing bladder discomfort and irritation, along with an elbow joint ache that was all occurring at the same time. In my internet search to see if others might have had these or similar symptoms, I found your article here. In doing a food log along with an elimination diet, I was down to just consuming bone broth protein shakes, and/or collagen hydrolysate in my coffee. For several days on this type of fueling, my bladder was severely sore to the touch, and a general burning heat-like sensation in my urethra. I needed to urinate every 40-60 minutes. And, when I sat on he toilet, the urine would just trickle out. I checked in with my Gynocologist to rule out a few other conditions I thought might have been causing these problems in my bladder and urinary tract. All tests were clear. So, that being the case I decided to look more closely at this collagen load I’d been taking in…I found your article and immediately eliminated the gelatins completely. Well, within just a 24-48 period, I was relieved. One year later I decided to add them back to my diet, and again the same exact symptoms occurred. So, I just wanted to post a comment to support your report here on the oxalate excess issue and the related problems that can occur with consumption of bone broth and collagen hydrolysate. By the way, for me, symptoms occurred at doses of 16-20 grams. Worse on the days I had double the dose.
LikeLike
I was using hydrolyzed collagen daily to try and help pain from OA. My orthopedic doctor had already recommended knee replacement. I wanted to avoid this and at least try to help my knees in a more natural way. Shortly after starting on the collagen I began to experience UTI symptoms and the urethra and bladder symptoms you describe. I was miserable, but had no idea to connect the two things. Numerous (6) antibiotics were used to try to eradicate the UTI. Symptoms continued. My GP referred me to a kidney specialist who discovered that I had a huge kidney stone. The stone was too large to be a candidate for lithotripsy so I ended up having to have kidney surgery. Near the very end of this ordeal I decided to check the oxalates in collagen and found out that I had been using the hydrolyzed collagen hoping to help my knees, and I had inadvertently done damage to my kidneys! I believe those selling these supplements should make the information on urine oxalates public and inform those at risk to avoid them. It’s the only responsible thing to do.
LikeLike
I have a 1972 book on organic acidurias that states that restricting protein doesn’t reduce urinary oxalate in hyperoxaluria. I imagine the usual turnover just increases if protein-deficient.
I tried to find a case study of kidney stones attributed to collagen and found this evidence that it’s well-tolerated in dialysis patients.
https://onlinelibrary.wiley.com/doi/full/10.1002/dat.20127
There is however a case study of ascorbic acid causing death by oxalate.
https://www.ncbi.nlm.nih.gov/pubmed/23882371/
LikeLike
(OK, no-one died in that case study, but I did see a fatal one mentioned on PubMed)
LikeLike
Indeed the article is insightful and well presented. I’m only want to restate, what I think was implied between the lines, that e-v-e-r-y-o-n-e is different and unfortunately you have to experiment to see how your metabolism responds. Overdoing anything will cause issues. Balancing out your nutrition, eating a variety of vegetables, vigorous exercise, regular hydration, lowering stress, and getting enough sleep are the basics that without give little hope unless you won the DNA lottery.
The inclusion of alcohol in your diet, gluten in the intestines, eating before bed, sugars, not hydrating etc. set the conditions for a host of possible problems that don’t need our help since we are kept alive artificially already. By that I mean most of us would have perished long ago without modern medical intervention from simple things ranging from impacted wisdom teeth, influenza, unclean water, infections, limited nutritional options, (bears) etc.
I have had kidney stones in the past, though none for many, many years now, yet I respond very well to (beef) bone broth. The energy I get from it is remarkable. I definitely am aware of purines and that overdoing bone broth is plain stupid. When I do take it (if I wish to be regular about including it in my diet) I only sip a bit several times a day. But I enjoy drinking only water and lots of it.
LikeLike
Alert, It is amazing this is not mentioned, but a common source of gelatin people are forgetting about is gummy type candies and any gummy at all is pure gelatin.They have to be more dangerous than bone broth by a long shot.
LikeLike
This is like a an anti meat propaganda article/study the amount of Oxalates in plant based food is much higher than regular meat diets, of course both broth is high in gelatin and should be avoided but there inst high amounts in regular meat, gelatin is worse than meat sources, look up hydroxyproline in meat, cant be so high compared to gelatin, anyway here are plant sources of oxalates almonds, amaranth, black beans, brazil nuts, beets, blackberries, buckwheat, carob chips, carrots, cashew nuts, cannellini beans, celery, chocolate, corn meal, dried apricots, cooked tomatoes, great northern beans, green peppers, hazelnuts, marshmallow root, milk thistle, navy beans, oil of oregano, okra, peanuts, pecans, pine nuts, pink beans, pinto beans, potato chips, potato flour, rice bran, rhubarb, sesame seeds and tahini, slippery elm bark, all soy, spinach, star fruit, sweet potatoes, teff (flour and whole grain), quinoa (whole grain), white bean flour, and yucca powder.
LikeLike
Hi Kevin,
Just curious. Where did you source your list of oxalates?
Thanks,
Polly
LikeLike